Front Oncol:一线TKI联合局部放疗可改善老年NSCLC伴有寡转移患者预后
2022-02-02 yd2015 MedSci原创
研究表明,对于老年NSCLC伴有寡转移患者,一线TKI联合局部放疗可改善患者预后,并且毒性可控。
近期,Frontiers in Oncology杂志上发表了一项研究成果,主要是评估在老年EGFR突变阳性的非小细胞肺癌(NSCLC)患者中伴有寡转移时一线使用EGFR-TKI联合局部增强放疗(LCRT)的疗效。
研究纳入确诊时伴有EGFR突变且寡转移性NSCLC(≦5个转移灶)老年患者。他们分别用一线TKIs单独治疗或与LCRT联合治疗。Kaplan-Meier评估无进展生存期(PFS)和总生存期(OS)。
2010年2月至2018年1月,共纳入122名符合标准的患者。其中,41.0% (n = 50)患者接受TKIs联合LCRT治疗(TKIs + LCRT组),59.0% (n = 72)患者接受TKIs单药治疗(TKIs单药组)。患者中位年龄72.5岁,超过75岁的患者占39.3% (n = 48)。大多数病人(n = 102, 83.6%)为腺癌,4.9% (n = 6)为鳞状细胞癌,54.9% (n = 67) 患者为21外显子L858R突变,59% (n = 72)患者有吸烟病史,63.9% (n = 78)有高血压,39.3%(48例)有糖尿病,28.7%(35例)有慢性阻塞性肺疾病(COPD),ECOG PS=0或1患者占52.5%(64例),N0-1期患者占46.7%(57例),T1-2期患者占51.6%(63例)。大多数患者(77.9%,n = 95)接受吉非替尼作为一线治疗。
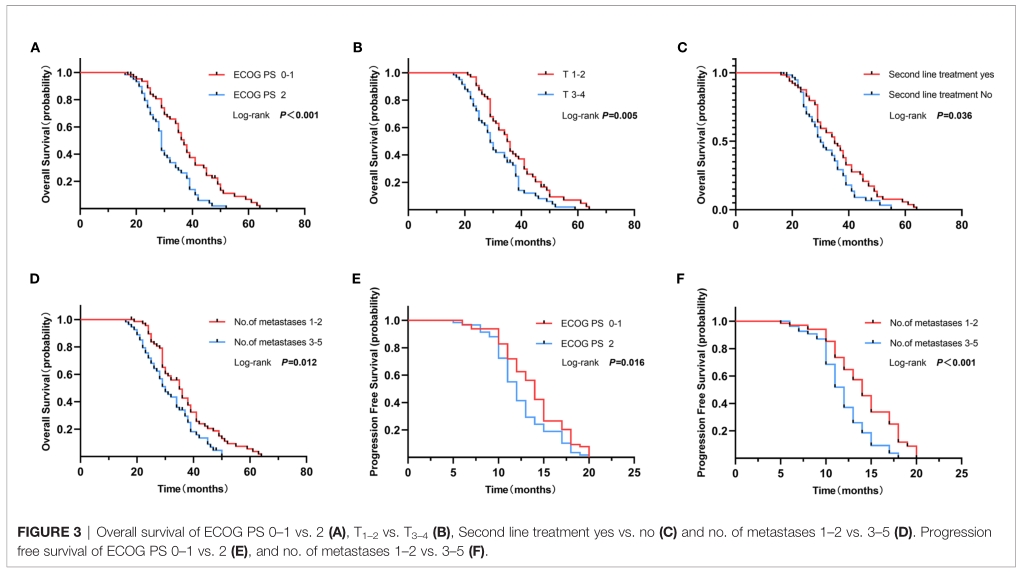
中位随访时间为34个月(7.0 ~ 64个月)。整个研究人群的mPFS为13个月,mOS为34个月(95%CI: 30.3-37.7)。TKIs + LCRT组中位PFS为17个月(95%CI: 15.37-18.63),明显长于TKI单药组(12个月;95%CI: 11.05 -12.95) (p<0.001)。TKIs + LCRT组中位OS为38个月(95%CI: 35.61-40.39), TKIs单药组中位OS为29个月(95%CI: 26.86-31.14) (p<0.001)。

多因素分析显示,LCRT、1 ~ 2个转移灶和良好的ECOG PS是较好的PFS的独立预测因子(p<0.001, p = 0.004和p = 0.027)。
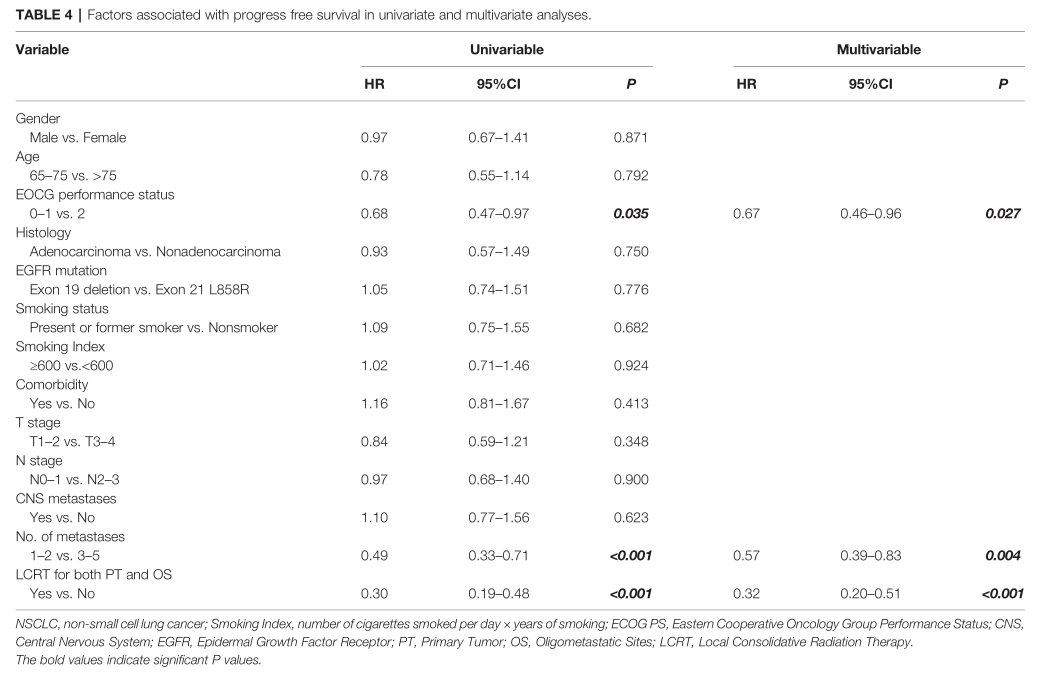
此外,LCRT、良好的ECOG PS和T1 -2期是更好OS的独立预测因子(p<0.001, p = 0.007和p = 0.007)。
在TKIs + LCRT组中,BED≧100Gy在单变量分析中与更好的OS和PFS相关(p = 0.004和p = 0.031)。

大多数患者发生1 - 2级毒性,治疗相关的死亡没有记录。
综上,研究表明,对于老年NSCLC伴有寡转移患者,一线TKI联合局部放疗可改善患者预后,并且毒性可控。
原始出处:
Hu X, Li H, Kang X, Wang X, Pang H, Liu C, Zhang J and Wang Y (2022) First-Line Tyrosine Kinase Inhibitors Combined With Local Consolidative Radiation Therapy for Elderly Patients With Oligometastatic Non-Small Cell Lung Cancer Harboring EGFR Activating Mutations. Front. Oncol. 12:766066. doi: 10.3389/fonc.2022.766066
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
85 举报
#患者预后#
104 举报
#TKI#
130 举报
#局部#
90 举报
置针回血在临床患者输液过程中是非
113 举报