FDA授予CAR-T癌症疗法CLBR001 + SWI019“快速通道称号”
2020-10-02 Allan MedSci原创
美国FDA已授予Calibr研发的新型“可切换”CAR-T细胞疗法CLBR001 + SWI019“快速通道称号”,以加快药物开发和审查。
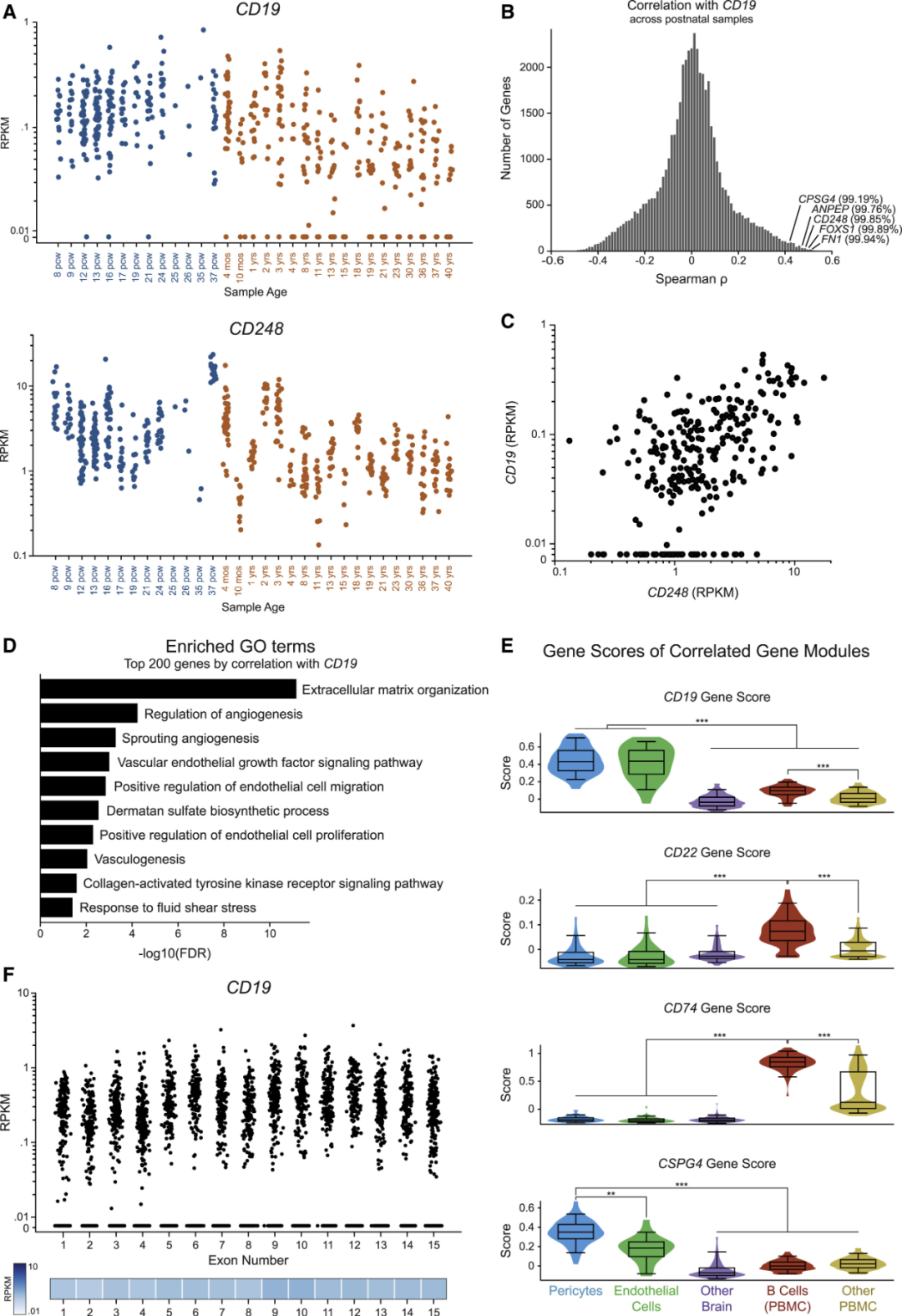
美国FDA已授予Calibr研发的新型“可切换”CAR-T细胞疗法CLBR001 + SWI019“快速通道称号”,以加快药物开发和审查。目前,该疗法正在评估作为B细胞恶性肿瘤的治疗方法,B细胞恶性肿瘤包括非霍奇金淋巴瘤和慢性淋巴细胞性白血病。

CAR-T细胞疗法CLBR001 + SWI019已开始招募受试者参加I期临床试验,旨在评估该细胞疗法的安全性和耐受性,这项研究正在美国的多个地点进行。
Calibr首席医学官Pamela Garzone博士说:“快速通道称号将使Calibr能够在相关研究上与FDA进行互动,例如适当的数据收集和研究设计,以支持该创新疗法的获批”。
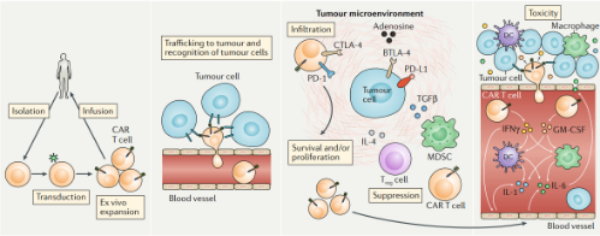
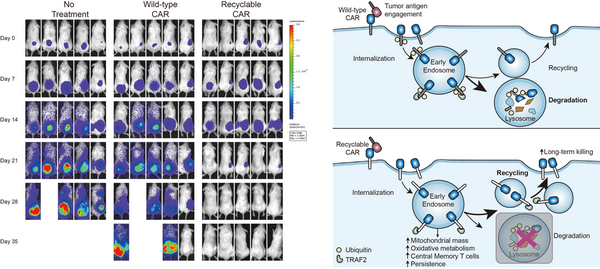
Calibr研究性的CAR-T细胞疗法利用患者自身的免疫细胞来治疗癌症,使这些细胞处于新型分子“开关”的控制之下,该“开关”试图减轻迄今为止可能威胁生命的副作用,这些副作用已阻碍了细胞疗法的使用。
Calibr的“可切换”CAR-T细胞疗法结合了一种称为“SWI019”的抗体,该抗体可作为“开关”,激活工程细胞(CLBR001),并指导它们与癌症靶标结合。这可以使医生对治疗有更多的控制,从而可以提供明显的安全优势。在临床前研究中,该方法被证明在消除肿瘤,同时控制因治疗而产生的细胞因子方面非常有效。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#癌症疗法#
102
#CAR-#
73
学习了,科技进步
167
😀
159
科技进步
150