Lung Cancer: 纳武利尤单抗(nivolumab)治疗既往治疗过的晚期NSCLC患者的2年生存:来自法国、德国和加拿大的真实世界研究
2021-06-30 yd2015 MedSci原创
真实世界中,纳武利尤单抗(nivolumab)治疗既往治疗过的NSCLC患者的OS与临床研究的类似,表明纳武利尤单抗在临床研究和临床实践中效果相当。
免疫检查点抑制剂已经广泛用于晚期非小细胞肺癌(NSCLC)的一线和二线治疗中。III期临床研究CheckMate 017 和 CheckMate 057都证实,对于既往治疗进展的NSCLC,二线纳武利尤单抗(nivolumab)较多西他赛明显改善患者的OS。两研究的综合分析,纳武利尤单抗较多西他赛降低患者的32%的死亡风险,HR=0.68 (95 % CI,0.59–0.78)。纳武利尤单抗组的中位OS为11.1个月(95 % CI, 9.2–13.1), 以及评估的1-, 2-, 4- 和 5-年OS率分别为48 %, 27 %, 14 %, 和13 %。但是我们知道,真实世界中的患者较临床研究中患者的临床特征更加的多样化。因此,来自法国、德国和加拿大的研究者,开展了一项真实世界研究,评估纳武利尤单抗治疗既往治疗过进展的NSCLC患者的疗效。相关研究成果发表在Lung Cancer杂志上。

患者来自两个前瞻性观察队列研究EVIDENS和ENLARGE, 以及来自加拿大的一个回顾性研究。患者≥18岁,分期为IIIB/IV NSCLC,接受纳武利尤单抗治疗前既往接受过至少一线的治疗。主要评估总体人群和亚组人群的OS。
纳入2585例患者,其中法国1235例 (47.8 %),德国881例(34.1 %)和加拿大469例 (18.1 %)。中位年龄为66岁;18.4%的患者年龄≥75岁; 62.5%为男性; 11.5%的患者ECOG PS≥2; 67.7%为非鳞状细胞癌。96.4 %患者接受过铂为基础的治疗。在非鳞状NSCLC中,EGFR突变状态为5.2%阳性,21.2%未知; 间变性淋巴瘤激酶(ALK)重排状态,0.5%为阳性,28.7%为未知。
总体人群的中位随访时间为17.5个月(range, 0–27)。总人群中位OS为11.3个月(95 % CI: 10.5–12.2) ;其中法国人群的中位OS为11.3个月 [95 % CI: 10.0–12.5]), 德国人群的为11.1个月 [95 % CI: 9.3–12.7]),加拿大人群的为11.9个月[95 % CI:10.7–13.5])。1年和2年的OS率分别为 49 %和28 %。
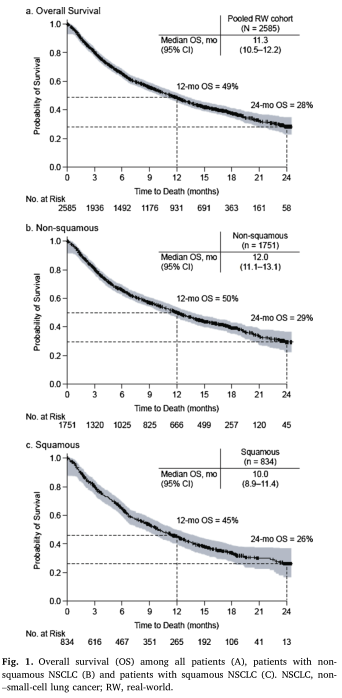
OS
总体人群非鳞状NSCLC患者的中位OS为12.0个月(95 % CI: 11.1–13.1),而鳞状NSCLC患者的中位OS为10.0个月(95 % CI: 8.9–11.4)。
亚组OS
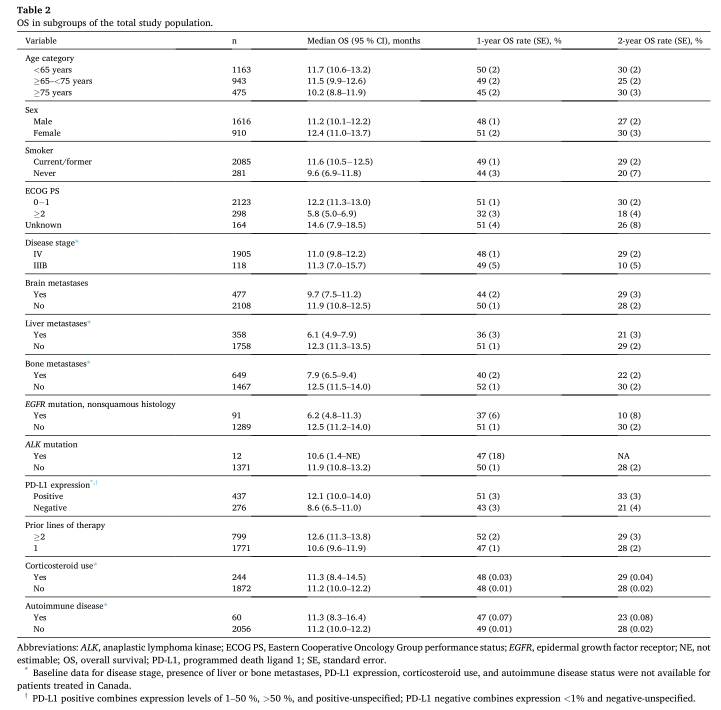
治疗初始ECOG PS为0 – 1的患者中位OS为12.2个月(95%CI:11.3—-13.0),评估的1年和2年OS率分别为51%和30%。而ECOG PS≥2的中位OS为5.8个月(95%CI:5.0—-6.9),评估的1年和2年OS率分别为32%和18%。PD-L1阳性表达阳性患者的中位OS为12.1个月(95% CI: 10.0-14.0), 评估的1年和2年的OS率分别为51%和33%;而PD-L1表达阴性的患者中位OS为8.6个月(95% CI: 6.5-11.0),评估的1年和2年的OS率分别为43%和21%。
无肝转移患者的中位OS为12.3个月(95% CI: 11.3 13.5),评估的1年和2年的OS率分别为51%和29%。肝转移患者的中位OS为6.1个月(95% CI: 4.9 7.9),评估的1年和2年的OS率分别为36%和21%。无骨转移患者的中位OS为12.5个月(95% CI: 11.5 14.0),评估的1年和2年的OS率分别为52%和30%。骨转移患者的中位OS为7.9个月(95% CI: 6.5 9.4),评估的1年和2年的OS率分别为40%和22%。
此外,中位OS在使用或不使用糖皮质激素的患者中相似(11.3个月 [95% CI: 8.4-14.5] vs 11.2个月[95% CI: 10.0-12.2]),两组评估的1年OS率分别为48%,2年OS率分别为29%和28%。自身免疫性疾病患者的中位OS为11.3个月(95%CI:8.3—16.4),无自身免疫性疾病患者的中位OS为11.2个月(95%CI:10.0—12.2);两组评估的1年OS率分别为47%和49%,2年OS率分别为23%和28%。
在单变量Cox分析中,肝转移(对比无肝转移,P<0.001)、骨转移(对比无骨转移,P<0.001)以及非鳞状NSCLC患者EGFR突变阳性的患者(对比突变阴性,P=0.0199)与较短的OS相关;而ECOG PS 0-1(对比2分,P<0.001)和PD-L1表达阳性(对比表达阴性,P=0.019)患者与较长的OS相关。

单变量预后因素
安全性仅在EVIDENS和ENLARGE研究中评估。大约三分之一患者报道了治疗相关不良事件(TRAEs),包括7.5% 3/4级的不良事件。大多数出现在治疗的第一年。中位时间为29天(15–85)。使用类固醇激素的患者中(n=244),36.9 % 患者报道了任何级别的TRAEs,没有使用的患者中为31.4 %。有或无自身免疫性疾病患者的任何级别TRAEs发生率分别为35%和31.9%。
综上,真实世界中,纳武利尤单抗(nivolumab)治疗既往治疗过的NSCLC患者的OS与临床研究的类似,表明纳武利尤单抗在临床研究和临床实践中效果相当。
原始出处:
Debieuvre D, Juergens RA, Asselain B, et al. Two-year survival with nivolumab in previously treated advanced non-small-cell lung cancer: A real-world pooled analysis of patients from France, Germany, and Canada. Lung Cancer. 2021 Jul;157:40-47. doi: 10.1016/j.lungcan.2021.04.022. PMID: 33980420.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#NIV#
92 举报
#SCLC患者#
72 举报
#mAb#
71 举报
#真实世界#
67 举报
#加拿大#
90 举报
#德国#
98 举报
#法国#
77 举报
#NSCLC患者#
75 举报
#晚期NSCLC#
0 举报
关注医学
99 举报