Investigative Radiology:光子计数探测器在增强乳腺CT中的应用
2022-09-12 shaosai MedSci原创
专用的乳腺计算机断层扫描(B-CT)可以看到与乳腺钼靶检查和断层合成术相当的微小钙化。此外,在B-CT中,不需要压迫乳房,这大大提高了患者的依从性。
 在乳腺癌组织筛查、机会性筛查和乳腺影像诊断中,最常用的影像学方法是乳腺钼靶检查。如果发现致密的纤维腺体组织,可以增加乳腺超声检查以进一步分析。最近的研究显示,通过在乳腺造影或断层合成检查中加入造影剂增强检查可以提高病变的诊断准确性,然而这两种检查都具有自身无法避免的弊端。另一种使用造影剂评估乳腺病变的检查技术是增强磁共振成像(CE-MRI),是检测乳腺癌的最敏感的乳腺检查方式。
在乳腺癌组织筛查、机会性筛查和乳腺影像诊断中,最常用的影像学方法是乳腺钼靶检查。如果发现致密的纤维腺体组织,可以增加乳腺超声检查以进一步分析。最近的研究显示,通过在乳腺造影或断层合成检查中加入造影剂增强检查可以提高病变的诊断准确性,然而这两种检查都具有自身无法避免的弊端。另一种使用造影剂评估乳腺病变的检查技术是增强磁共振成像(CE-MRI),是检测乳腺癌的最敏感的乳腺检查方式。
专用的乳腺计算机断层扫描(B-CT)可以看到与乳腺钼靶检查和断层合成术相当的微小钙化。此外,在B-CT中,不需要压迫乳房,这大大提高了患者的依从性。与乳腺MRI相比,B-CT是一种快速的检查手段,可以在有MRI禁忌症的患者中进行。
近日,发表在Investigative Radiology杂志的一项研究介绍了一种新的专用造影剂螺旋B-CT(CE-B-CT)的首次临床活体检查结果,以同时对ST造影剂增强的病变和微小钙化进行检测,提供了B-CT中病变大小与手术样本的组织学工作的比较,并计算了增强B-CT检查中所描述病变的信噪比(SNR)。
本研究纳入了12名在乳腺钼靶检查或B-CT中发现可疑乳腺病变的女性进行了增强螺旋B-CT和辅助超声检查。并获得了所有病变活检证明的诊断和手术切除后的组织学结果,包括癌症/原位癌的大小。同时对肿瘤、腺体组织和脂肪组织的信噪比和对比度进行了评估。
在12名患者中,发现15个可疑病变,14个是恶性的,1个良性病变对应的是慢性炎症。所有病变都表现出强烈的造影剂摄取,信噪比为119.7±52.5,腺体组织和乳腺癌病变之间的信噪比为12.6±5.9。B-CT测量的浸润性肿瘤的大小与组织学大小相比有显著的强相关性R=0.77(P<0.05),而与瘤周原位导管癌的大小相关性不显著R=0.80(P=0.11)。

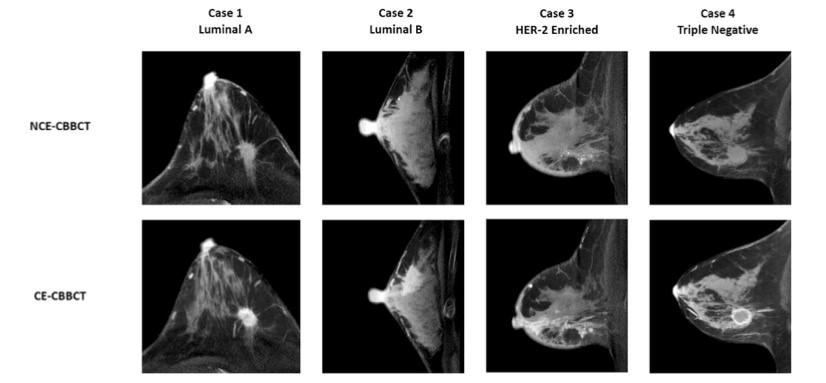
图 54岁患者,患有浸润性导管癌并伴有原位导管癌(DCIS),肿瘤在应用造影剂后显著增强(箭头)
本研究表明,CE-B-CT显示了乳腺癌和周围腺体组织之间的高对比度,提示该技术是一种十分具有临床前景的癌症检测和分期技术,可以对ST病变和微钙化进行精确显示,比乳腺MRI有更大的临床优势。
原文出处:
Nicole Berger,Magda Marcon,Jann Wieler,et al.Contrast Media-Enhanced Breast Computed Tomography With a Photon-Counting Detector: Initial Experiences on In Vivo Image Quality and Correlation to Histology.DOI:10.1097/RLI.0000000000000863
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EST#
171
学习
197
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
98
认真学习~~
110
#IgA#
124