Movement disorders:SCA3的轴向和径向共济失调,如何随时间变化
2022-07-11 Freeman MedSci原创
SCA3患者的轴向和径向共济失调的时间动态差异如何
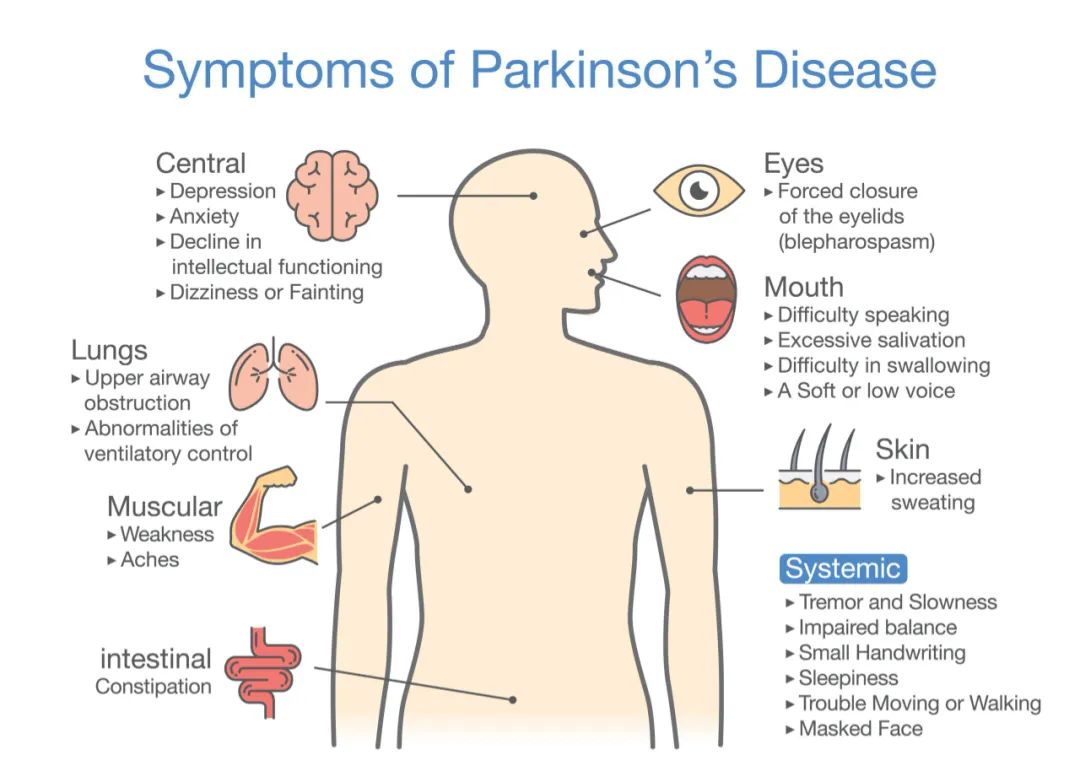
脊髓小脑共济失调3型(SCA3)是一种破坏性的神经退行性疾病,主要影响小脑和桥脑深部核团、基底神经节和脊髓。尽管发病率有很大的地域差异,但它被认为是全世界最常见的显性遗传性共济失调,估计占受影响家庭的20%-50%。 SCA3是由ATXN3基因中一个不稳定的多聚谷氨酰胺编码的CAG重复扩展引起的,它引发了一系列复杂的事件,最终导致广泛的神经元损失。
图1: 论文封面图
过去15年见证了该领域的重要发展,包括共济失调评估和评级量表(SARA)的构建和验证,临床前疾病阶段的定义,欧洲和美国研究联盟的建立,以及大规模纵向研究的实施。 然而,这些努力主要集中在总体共济失调严重程度的进展上,如SARA总分的年度变化,而没有具体评估单一SARA项目或将轴性与阑尾性项目分组的子分数的时间动态。
最近在弗里德里希共济失调(Friedreich Ataxia)中描述了轴性和径性体征的自然历史差异,在一项涉及SCA3患者的单中心研究中也注意到了这种差异。对项目得分的仔细调查不仅可以提供有关退行性小脑疾病临床演变的更详细的信息,而且还可能对SARA作为治疗试验中(主要)结果测量的应用产生重要影响。
藉此,荷兰拉德堡德大学的Roderick P.P.W.M. Maas等人, 结合使用来自SCA3突变携带者的大型国际队列的横断面和纵向数据,试图研究SARA及其各个项目的进展模式,并特别关注轴向与阑尾的分值。此外,还研究了人口统计学、临床和遗传因素是否与轴向和阑尾分值的进展率有不同程度的共线性,以及SARA项目得分的年度变化是否与SCA3的相应功能测量的变化相关。
这个研究涉及11个欧洲和2个美国的前瞻性多国队列研究中,对223名SCA3患者的SARA评分进行了纵向测定,并在1年后进行了随访评估。
他们发现:SARA得分从10分增加到20分主要是由轴向和语言项目驱动的,而阑尾项目的贡献明显较小。
追指(finger-chase)和鼻指(nose finger)测试的分数不仅在基线上显示出最低的变异性,而且在随访中也显示出最小的恶化。与全套SARA项目相比,省略这两项测试会使治疗试验的样本量要求降低。
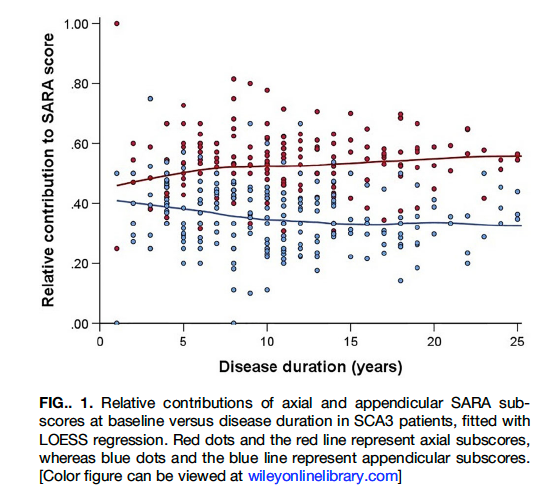
图2:论文结果图
性别与SARA总分和阑尾分的变化有关,但与轴向分的变化无关,男性的进展明显更快。尽管个体间存在相当大的差异,但病程超过10年的受试者的SARA评分的平均年进展率比发病后10年内的受试者高约3倍。
该研究的重要意义在于:为SCA3患者的轴向和径向共济失调的时间动态差异提供了证据,这将有助于为临床试验的设计和新的(特定病因)结果测量方法的开发提供信息。
原文出处:
Differential Temporal Dynamics of Axial and Appendicular Ataxia in SCA3. _Movement Disorders_. Published online 2022:12.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#ERS#
169 举报
#Dis#
105 举报
#disorder#
86 举报
#Disord#
108 举报
#disorders#
119 举报