Diabetic Med:1型糖尿病青少年的治疗
2018-10-24 MedSci MedSci原创
为了更好地了解糖尿病患者自我护理的驱动因素和障碍,近日,国际杂志 《Diabetic Med》上在线发表一项关于1型糖尿病青少年的治疗偏好-使用离散选择实验模型的国家研究。使用离散选择实验模型对全国范围内1型糖尿病的青少年中进行测试。 在一小部分目标人群中(年龄在15至<18岁且患有1型糖尿病的青少年)构建并测试了调查工具。然后通过瑞典儿科糖尿病质量登记处SWEDIABKIDS识别瑞典
为了更好地了解糖尿病患者自我护理的驱动因素和障碍,近日,国际杂志 《Diabetic Med》上在线发表一项关于1型糖尿病青少年的治疗偏好-使用离散选择实验模型的国家研究。使用离散选择实验模型对全国范围内1型糖尿病的青少年中进行测试。
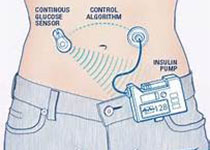
在一小部分目标人群中(年龄在15至<18岁且患有1型糖尿病的青少年)构建并测试了调查工具。然后通过瑞典儿科糖尿病质量登记处SWEDIABKIDS识别瑞典属于该目标组(N=2112)的所有个体,并且发送邀请以回答在线问卷。研究共获得了对431个人进行了离散选择实验分析的有效响应。
研究结果表明,纳入的受访者在年龄和糖尿病病程方面与非参与者没有统计学差异,但年轻女性进入研究较多,参与者(平均)HbA 1c值明显低于非参与者。参与者认为非严重低血糖事件(白天和夜晚)和高血糖事件都是不可取的。女性受访者中,避免体重增加,甚至实现体重减轻是最重要的方面,她们愿意以大幅度的血糖控制[13 mmol / mol(1.2%)]进行换取,以避免体重增加3 kg。
鉴于现实生活中的两难困境,这些回答可能会为受访者优先考虑的方面提供有用的提示。对于治疗效果,按性别划分的分层很重要,而治疗管理方面应根据治疗类型进行分层,因为这些方面是密切相关的。
原始出处:
G. Forsander, S. Stallknecht, U. Samuelsson,et al. Preferences for treatment among adolescents with Type 1
diabetes: a national study using a discrete choice experiment model
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Diabetic#
66
#BET#
66
#DIA#
102
#Med#
78
谢谢MedSci提供最新的资讯
137