BJC:S-1加顺铂联合同步放疗治疗局部晚期不可切除的非小细胞肺癌
2018-09-30 MedSci MedSci原创
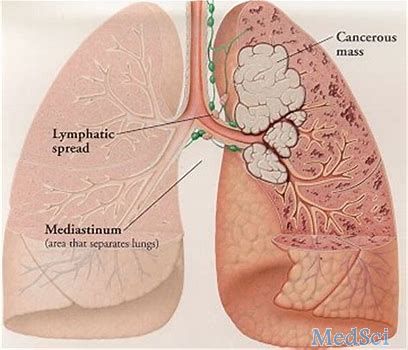
非小细胞肺癌是世界范围内肿瘤致死的主要原因之一。以顺铂为基础的放化疗是不可切除的局部晚期非小细胞肺癌(NSCLC)的标准治疗方案。BJC近期发表了一篇文章,报道了将两种化疗方案与同步放疗相结合的临床试验的结果。
原始出处:
Tomonari Sasaki, Takashi Seto,et al. A randomised phase II trial of S-1 plus cisplatin versus vinorelbine plus cisplatin with concurrent thoracic radiotherapy for unresectable, locally advanced non-small cell lung cancer: WJOG5008L. BJC.September 2018 doi:https://doi.org/10.1038/s41416-018-0243-2
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#局部晚期#
109 举报
#非小细胞#
124 举报
#铂#
82 举报
#局部#
121 举报
#S-1#
92 举报
很好的学习机会
109 举报
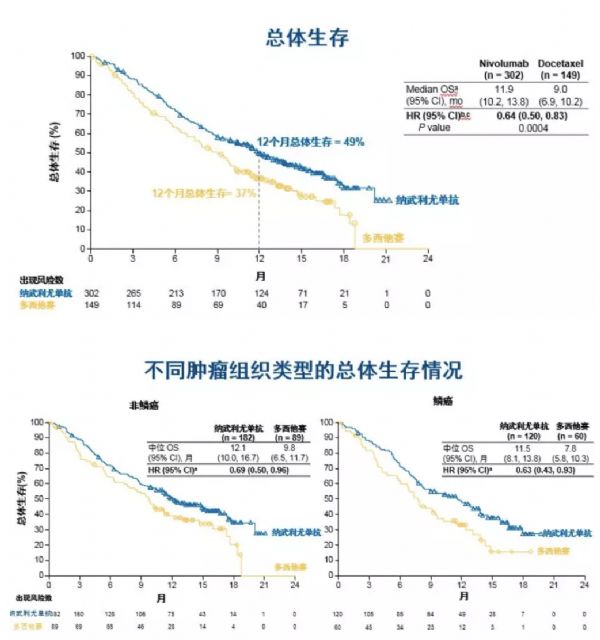
死亡的危险比(HR)为0.85。
103 举报